Admin
May 14, 2021
Epidemiology, smart technology, and the public health insights we flush down the drain

As the world looks for ways to manage the COVID-19 pandemic, researchers and epidemiologists are turning to the sewers for answers. With the help of smart technologies, our shared waste could hold the key to community health both now and in the future.
Field engineers from Kando, a wastewater intelligence firm, collect a sewage sample from one of the company’s automated smart samplers
In one minute:
During a cholera outbreak in 1854, John Snow plotted cases on a map of London, tracing the cause of infection to a sewage-contaminated water pump and proving two things: 1) Cholera is a waterborne disease, and 2) by understanding the networks communities share, we can better understand public health.
Modern epidemiology was born.
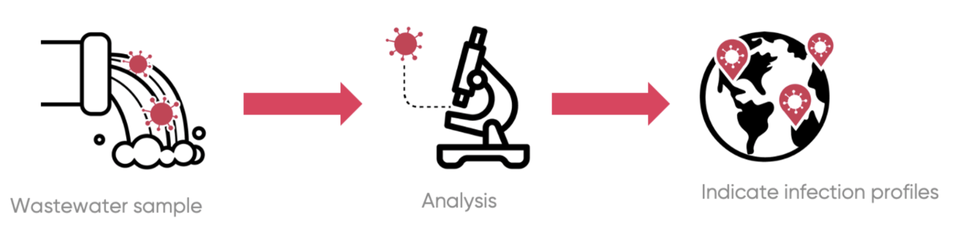
Today, researchers are turning to the sewers to track the spread of COVID-19 infections, taking samples of raw sewage and testing it for virus RNA shed by those infected.
By monitoring the concentration of viral traces in wastewater, public health officials are able to identify outbreaks and model their severity without needing to test people individually.
While not a direct replacement for individual testing, wastewater-based epidemiology (WBE) can play an important role in monitoring long-term public health patterns with minimal inconvenience.
WBE uses the sewer networks and the wastewater we flush away everyday, with no need for specialist testing facilities or extraordinary public engagement.
With COVID-19, infected persons shed virus RNA even before developing outward symptoms. Using WBE, outbreaks can be identified several days earlier than is usually possible with individual testing, but sample timing is crucial to maximising its effectiveness.
There are all sorts of things other than human waste that can impact wastewater’s viral load. Taking samples when faecal loads are highest and other contaminants are predictable is key to getting a sample that reflect a population’s infection profile accurately.
Technologies, such as those provided by wastewater intelligence specialists Kando, exist that automatically draw samples from the sewers when conditions are right, and signal to local authorities that there’s a sample ready to be collected, giving them the best chance of staying one step ahead of the virus’ spread.
With the right technological support, wastewater-based epidemiology can play a vital role in monitoring for and containing viral outbreaks as they happen, helping the world come out of this pandemic and respond effectively to the next.
In 5 minutes:
Water and sewage have been at the centre of epidemiology from its outset. As cholera decimated 19th-century London, everyone, including the scientific community, was blaming the city’s ‘noxious air’. Fortunately for history, a local doctor by the name of John Snow thought a little differently.
During an outbreak in 1854, he plotted cholera cases on a map, tracing the disease back to a single water pump on Soho’s Broad Street, modern day Broadwick Street. The pump was disabled by removing the handle and the cases fell away.
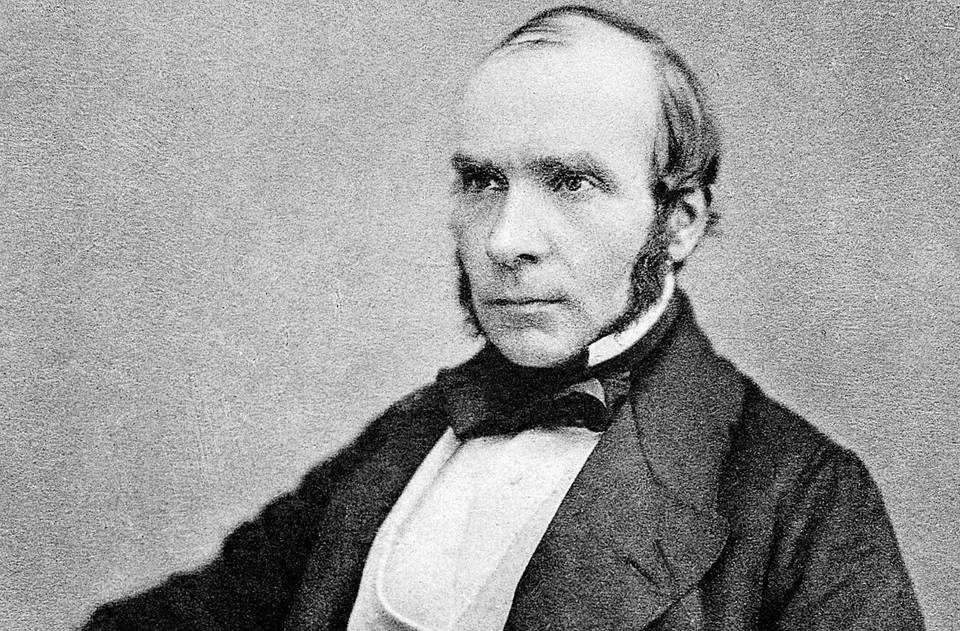
Dr John Snow, one of the key figures in the foundation of modern epidemiology.
Dr Snow had not only shown cholera to be waterborne, but that by understanding the networks communities shared, you could understand the diseases that ravaged them. His work was a significant step in modern epidemiology’s development.
Counting the number of virus particles present in wastewater gives an instant snapshot of an area’s infection status.
After some digging — literally in this case — the cause of the Broad Street cholera outbreak was found to be a cesspit, dug less than a metre from the public water well. Faecal bacteria had seeped into the supposedly potable supply, ultimately leading to the deaths of more than 600 people over just a few days.
Thanks to Dr Snow’s work, cholera is no longer the threat it once was in London, but the link between understanding our wastewater and understanding the diseases that infect our lives has never gone away.
Today, researchers are turning to the sewers to track the spread of COVID-19 infections, taking samples of raw sewage and testing it for viral RNA.
The principle is analogous to children pulling a bucket of water from a pond to see what creatures are swimming in it. The difference is, rather than a picturesque pond or a natural river, the samples scientists are analysing are taken directly from the sewers, and rather than water boatmen or shrimp, they’re scooping up a concoction of a community’s waste.
What they’re particularly interested in is faecal matter. People infected with SARS-CoV-2 (the virus that causes COVID-19) shed viral RNA in their stool. Counting the number of virus particles present in a sample gives an instant snapshot of the state of covid infection in an area.
At the peak of the UK’s second wave of infections in January, a litre of sewage water in the sewage network of any large city is estimated to have contained between a million and ten million virus particles, depending on the severity of the outbreak in the local area.
That means that by examining wastewater, you can not only identify if a virus is present in a community, but also estimate an outbreak’s intensity.
An obvious question to ask is, ‘why is this better than testing individuals? Surely the results are similar.’
The simple fact is that stools are easier to deal with than people; testing the wastewater people produce on a daily basis enables a far more comprehensive overview of an entire community’s health, while avoiding the biases inherent in programmes that test individual people.
To test people, you have to set up testing centres and have staff to work them. You have to tell people what to do and make sure every procedure is carried out perfectly every time, and even then, you can only test the people who come to the station in the first place.
Sampling the wastewater is more egalitarian, less invasive and disruptive, and easier to anonymise.
Voluntary, personal testing will inevitably lead to some groups being disproportionately over or under represented in any given test sample. Individuals are more or less conscientious. Some can take time off work more easily than others. They may live closer or farther away from a testing centre. Whatever the reason, bias is almost unavoidable.
But everyone goes to the toilet, and most toilets in the developed countries are connected to integrated sewage systems.
What’s more, for COVID-19, infected persons start shedding virus RNA before they develop outward symptoms, so by monitoring the wastewater, you can see an outbreak in its very earliest phase, and act to contain it before it spreads too widely.
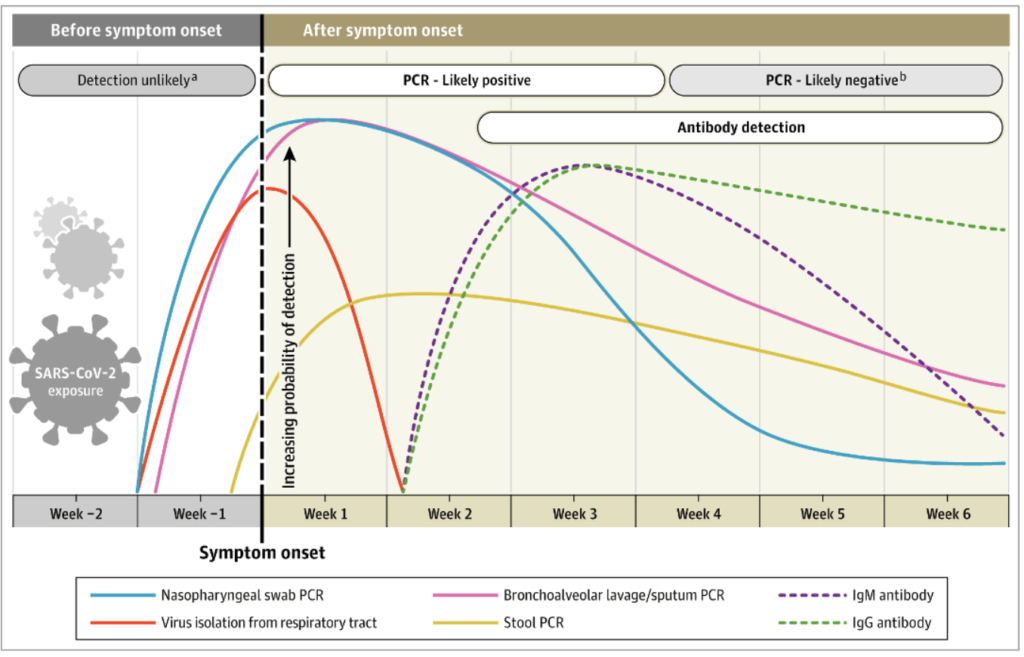
The pattern of infection and detection. Although nasopharyngeal swab PCR testing can detect COVID-19 cases slightly earlier than stool PCR, stool tests still identify infection before symptoms start to show. As most people don’t get tested until developing symptoms, stool PCRs can buy vital time to contain outbreaks.
Your wastewater contains the data.
We just need to extract it so that you can optimize your operations.
Contact us and a member of our team will get back to you as soon as possible.